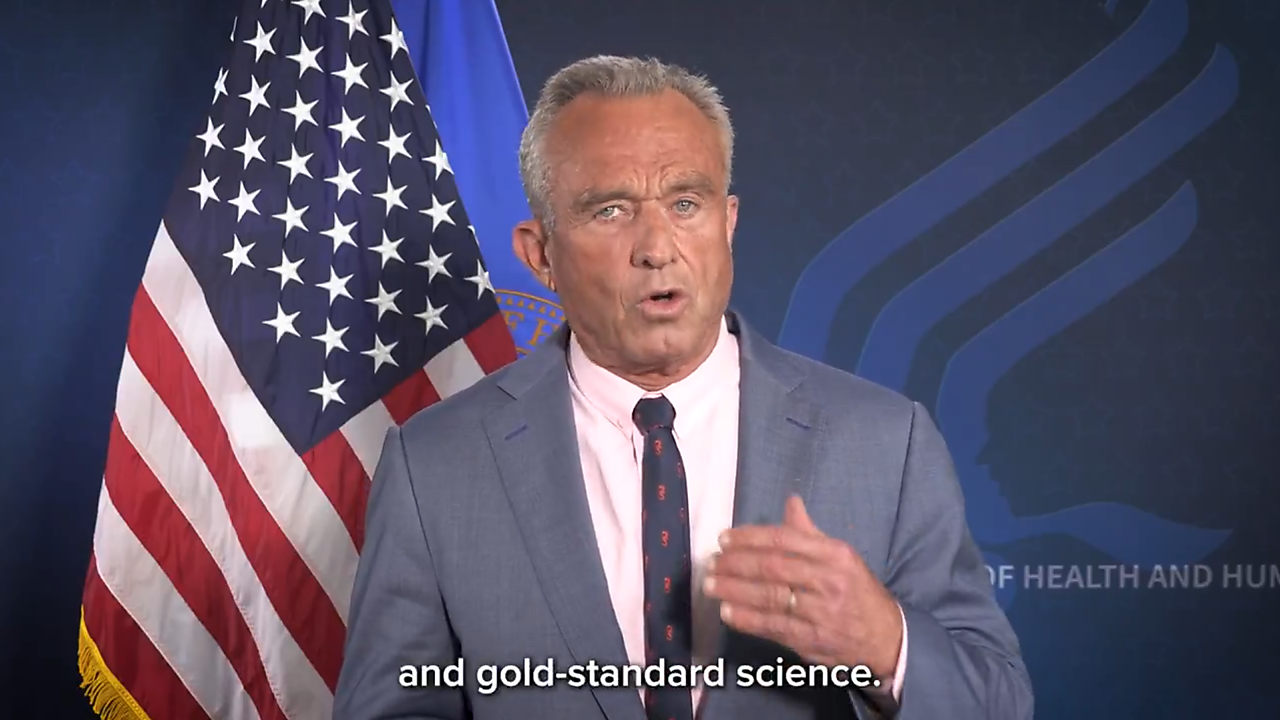
Last June, Secretary of Health and Human Services Robert F. Kennedy Jr. dissolved the 17-member Advisory Committee on Immunization Practices (ACIP), which advises the Centers for Disease Control and Prevention on immunization policy. Shortly afterward, he appointed eight new members to the panel, some of whom have held controversial and skeptical views on vaccines and vaccine safety. The panel has not yet returned to its original size of 17 members.
In announcing the dismissal of the committee members, Kennedy claimed the panel was filled with conflicts of interest. However, yesterday the Journal of the American Medical Association published a “Research Letter” authored by scholars at the University of Southern California and the Center for Science in the Public Interest that argues conflicts at ACIP have been at historic lows for years, and ACIP members have not been receiving income from vaccine makers.
Senate HELP Committee Chair Bill Cassidy, MD (R‑LA), later called on Secretary Kennedy to postpone the recently formed committee’s meeting, citing concerns that some members were biased against vaccines in general and mRNA vaccines in particular. He was unsuccessful.
In June, the committee voted 5–1, with one abstention, to recommend that seasonal influenza vaccines for adults, children, and pregnant women be administered only in single-dose, thimerosal-free formulations, effectively eliminating multidose vials containing thimerosal. Critics argue this decision ignores the strong scientific consensus that thimerosal is safe at the concentrations used and may limit vaccine access due to higher costs and decreased supply.
Science or Politics? The Debate Over Vaccine Recommendations
In a June 26 statement, the Infectious Diseases Society of America (IDSA), which represents physicians, scientists, and other health professionals specializing in infectious diseases, criticized the ACIP meeting as “politicized, chaotic, and not transparent.”
Robert H. Hopkins, Jr., MD, the Medical Director of the National Foundation of Infectious Diseases, warned, “The [committee’s] process we witnessed instills doubt rather than builds confidence and calls into question the legitimacy of the votes taken, including the vote on thimerosal in influenza (flu) vaccines.”
The “Partnership to Fight Infectious Disease, which represents “patients, providers, community organizations, academic researchers, business and labor groups, and infectious disease experts,” expressed fears that bypassing the traditional, rigorous vetting for ACIP members jeopardizes the committee’s credibility and public confidence.
Yesterday, the American Academy of Pediatrics (AAP) released COVID-19 immunization recommendations that contradicted the new HHS guidance that Secretary Kennedy announced last May. The AAP recommended that shots be given to children aged six months to two years. This was the first time in 30 years the AAP openly disagreed with government guidelines.
Also yesterday, an ad hoc group of 24 doctors, researchers, and public health experts, called the Vaccine Integrity Project (VIP), led by Michael Osterholm, MD, a University of Minnesota epidemiologist, held a public meeting where they reviewed thousands of peer-reviewed scientific articles and hundreds of studies and clinical trials. They concluded that the research shows flu, COVID-19, and RSV vaccines are safe and effective for children, pregnant women, and immunocompromised people.
Osterholm reportedly said there is no scientific reason to justify Secretary Kennedy’s decision to no longer recommend the COVID vaccine for children or healthy pregnant women. The VIP has received substantial financial backing from Alumbra, a foundation that the widow of Walmart heir John Walton founded.
HHS spokesperson Andrew Nixon, criticizing VIP, told Axios, “America doesn’t need another unaccountable group of former officials circling the wagons to protect outdated narratives.”
Why Government Guidance Shouldn’t Be Mandatory
The dispute over ACIP highlights a larger reality: when government panels make recommendations on medical practice, those statements seldom stay optional. They turn into mandates in all but name.
The issue isn’t whether thimerosal is safe or whether children should get COVID shots. It’s that these questions shouldn’t be decided by a politicized government committee at all.
Regardless of who is right here, I welcome these developments. As I have written here, here, and elsewhere, regarding prescribing medications to manage pain, government guidelines—disclaimers notwithstanding—amount to de facto mandates.
In a Public Comment on the CDC’s pain management guidelines revision in 2022, I wrote:
This disclaimer is good as far as it goes. The realities are that when the CDC issues guidelines, they become de facto edicts. As occurred after the CDC released the 2016 Guideline, lawmakers, pharmacies, third-party payers, and state and local organizations or entities will interpret the Guideline as the “official” standard of care. Therefore, while the disclaimer is laudable, it will not have the intended effect. The only effect it will have is to assure the CDC is not held responsible for misapplication of the revised guideline.
Furthermore, it is inappropriate for a government agency such as the Centers for Disease Control and Prevention, which is subjected to special interest pleading and political pressures, to establish “standard or care” or “best practices” guidelines. That has always been a principal function of medical specialty organizations, such as the American College of Physicians, American College of Surgeons, American Academy of Pediatrics, etc. These organizations are non-profit, non-governmental bodies that were created specifically to evaluate the evidence and provide education and practice guidance to practitioners in their specialty. To do so, they establish working committees of active clinicians, many of whom are also educators and researchers, and all of whom are aware of the nuances of clinical medicine and the variability of clinical circumstances. Such committees are better able to adjudicate pronouncements and assertions by various participants in the field
In a June 10 blog post about Secretary Kennedy’s dismissal of the ACIP committee members, I emphasized the importance of distinguishing between public health and personal health:
Governments have a legitimate role in addressing public health challenges…. In the realm of public health, this [harm] principle underlies efforts to control infectious diseases and manage environmental pollution. Therefore, it is appropriate for the government to engage in public health policy, particularly in areas where the actions of some may threaten the lives and safety of others. Too often, government-directed health policy today focuses on personal health issues, which individuals can assess and manage on their own, consulting experts as necessary…. While vaccines like tetanus and shingles are clearly personal health choices, others—such as influenza or even COVID-19—may blur the line, depending on the context and population-level risk.
Breaking the Monopoly on Medical Truth
Scientific knowledge is a work in progress. It is not a dogma. Scientists examine the evidence, debate its reliability and significance, and argue over conclusions. That’s the way knowledge advances.
The advent of professional and scientific societies challenging government recommendations and debating them in the public square is a good thing. The government shouldn’t have a monopoly on the truth—scientific or otherwise. Hopefully, we are witnessing the beginning of the breakup of that monopoly.
Breaking up the government’s monopoly on medical truth doesn’t weaken science—it strengthens it by restoring debate, humility, and the freedom for patients and doctors to make their own decisions.